Balance is a skill you don’t think about until you really need it — like when you lose your footing and have to perform an exotic improv dance to keep from hitting the ground. But don’t wait until your sense of balance fails before you give it proper attention. As we age, balance can sharply decline, often with little warning. An exercise program called BEEP can help.
How you keep your balance
While keeping proper balance may seem simple, it involves a complex system with many moveable parts. Whenever you move, your eyes and brain process information about your surroundings. Your feet detect changes in the terrain. Your arms swing to keep you stable, and your lower-body muscles and joints generate rapid power so you can move forward, stop, and change directions.
Unfortunately, this system works less effectively over time. The sensation of our bodies moving through space is not as crisp, and information travels more slowly between the body and brain. Muscles become weaker, and joints lose flexibility.
Any breakdown in your balance system increases your risk of falls, which can cause hip fractures, broken bones, and head injuries.
“Doing more balance exercises and activities can keep your sense of balance in good shape, but you also want to focus on multifaceted movements that work on all the elements of your balance system,” says Dr. Brad Manor, associate director of the Mobility and Falls Translational Research Center with Harvard-affiliated Hebrew SeniorLife.
There are many kinds of balance exercises. Science has not tapped any specific ones as the best; however, some have stood out in many balance-related studies.
For instance, a 2016 study in the journal Gerontology and Geriatric Medicine found that a specific Balance-Enhancing Exercise Program (called BEEP for short) improved balance skills among adults ages 60 to 80. Study participants did better on both solid and uneven surfaces, and increased their walking speed and overall confidence.
Focus on three exercises to improve balance
The BEEP program focused on three exercises: squats, heel and calf raises, and one-legged standing. “These types of exercises increase both the physical and cognition skills needed for better balance,” says Dr. Manor. “Plus, they mimic movements of everyday life.”
He recommends adding these to your regular workouts or doing them daily on their own.
Squats. Stand with your feet shoulder-width apart. Bend your knees and imagine you are sitting down on a stool. Lower down until your thighs are parallel to the ground, or as far as is comfortable. Keep your weight on your heels. Extend your arms forward or place your hands on a chair, counter, or table for stability. Pause for a second or two, then rise back to the starting position. Do this up to 10 times.
Heel and calf raises. Stand with your arms crossed over your chest and lift your heels, so you rise up on your toes. Hold this position for up to 10 seconds, or as long as possible, and then lower your heels. Do this five to 10 times. If you need support, hold on to a door frame, a table, or another sturdy object. You also can place your hands flat on a wall.
One-legged standing. Stand tall and place your hands on your hips or hold on to a table or chair for stability. Then raise one leg, so your foot is about six to 12 inches above the floor. Keep your gaze straight ahead. Hold for 20 to 30 seconds. Repeat on the other leg. Go back and forth three to five times.
You also can perform these exercises with your eyes closed to work on coordination and concentration. Another option is to “distract” yourself by doing unrelated cognitive tasks — count backward, name words that begin with the same letter, or make a mental supermarket list.
“Balance is definitely a use-it-or-lose-it skill,” says Dr. Manor. “But if you work on your balance continuously, you are almost guaranteed to see improvements.”
About the Author

Matthew Solan, Executive Editor, Harvard Men's Health Watch
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s … See Full Bio View all posts by Matthew Solan
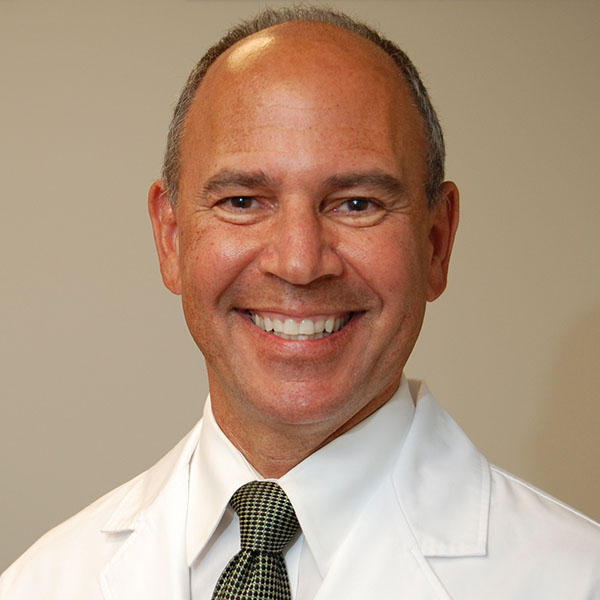
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD